- En /
- Aesthetic surgery /
- Gynecomasty
GYNECOMASTY
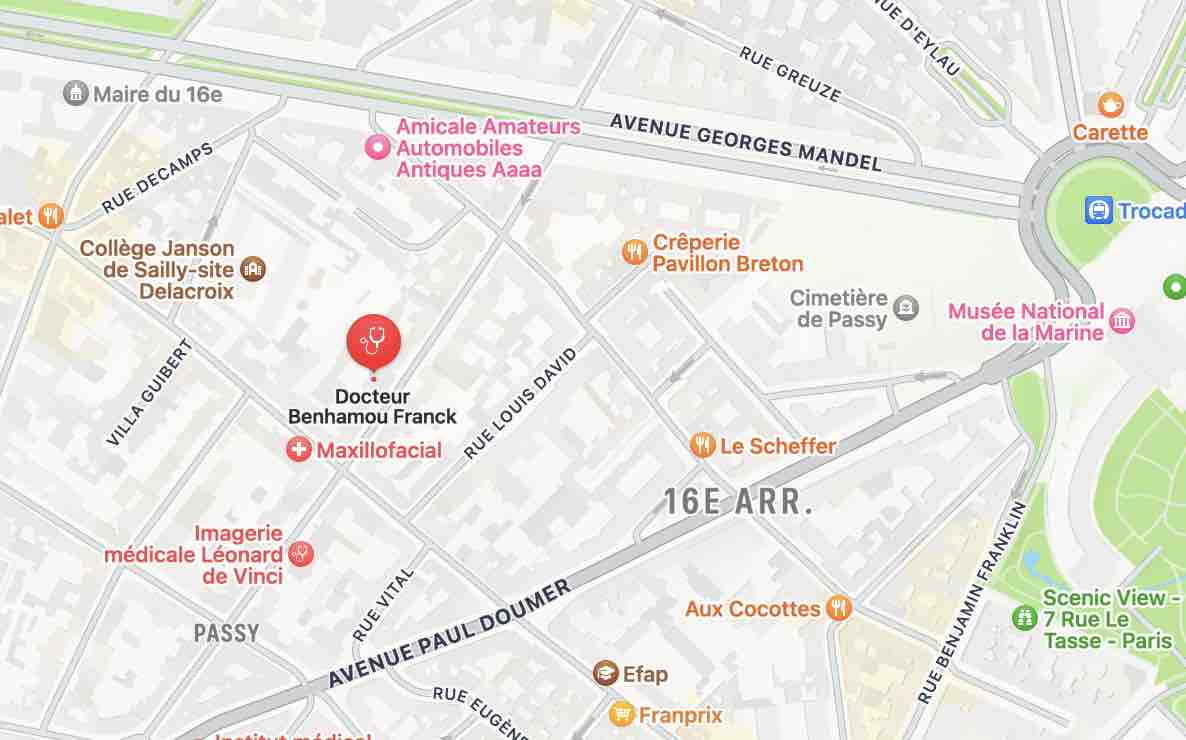
- Written by Dr. Franck Benhamou
- Publication date 21 novembre 2024
- Updated date 14 octobre 2025
The Surgery of Gynecomasty
The surgery is meant to reduce the excess of volume of the gland and fibro-fat. The goal is to remove the excess of gland and fat (and in some case, of skin).
According to the degree of gynecomasty, two types of scars are possible:
- Usually, a liposuction is enough. Sometimes, it can be associated with a lower hemi-areola incision for the exeresis of the retro-areola core.
- In some other cases, an incision in the shape of a reversed T is performed around the areola or in the under-breast fold plus areola incision.
A pre-op evaluation is necessary before surgery as well as hormonal assessment and sometimes mammagraphy and / or echography.
Classical general anesthesia is performed. An anaesthetist doctor must be consulted at least 48 hours before surgery.
A one day hospitalization is usually sufficient.
About the surgery of Gynecomasty:
Surgery may last from one to one and a half hour if a complementary associated surgical act is necessary.
If only liposuction is performed, no drainage is necessary. Only in the case of a T shaped scar or under mammary incision, a drain (redon) is placed. So that blood and collected secretions may be evacuated, it is usual to leave a drain (redon) until the day after surgery.
Stitches will be removed from one to two weeks after surgery.
Post surgery effects:
This type of surgery usually is not painful.
After 24 hours, the first dressing is removed and replaced by a compressive bandage giving a good support. Ecchymosis will fade away in one to two weeks.
A one week convalescence must be considered and it is not advised to practice any sport activity until complete closing up, i.e. about one month after surgery for the T shaped incision.
Result will be quickly visible. It will be final only after a span of two to three months. This delay is necessary for reduction of the edema. The changes in time depends upon variations of weight.
Complications
After any kind of surgery, complications may occur, some due to the medical and / or anesthesia act, others particular to gynecomasty. Good security practices can limit risks but do not suppress them. Some risks, very exceptional hopefully, cannot be anticipated and may endanger the vital or functional prognosis (emboly, paralysis, septicemy…).
Anesthesia carries its own complications which will be explained to you when you meet with the anaesthetist doctor.
Risks specific to gynecomasty surgery
Even if the post surgery effects are usually very simple, some of the possible complications linked to gynecomasty must be known :
Bad evolution of scars: it is normal that scars get thicker and redder during the first month. This aspect, linked to the inflammatory reaction of any closing up, takes twelve to eighteen months to get better and stabilize. Closing up may follow an abnormal evolution with thickening and swelling going on over a year. We speak of hypertrophic, even cheloid scars (they occur more often on black skins). They may occur in an unpredictable fashion and require specific treatment. It must be known that scars usually fade away and get less visible but don’t disappear.
Infection: most often, contamination of a wound, scar or drain opening is not serious. Very scarcely are antibiotics necessary, but infection can be treated with frequent dressings.
Haematoma: post surgery bleeding is almost unavoidable and gives way to ecchymosis (bruises) on the skin for one to two weeks. It may cause an haematoma with swelling and painful tightening. Sometimes there is a need for additional intervention to evacuate the haematoma and treat its causes. If bleeding is important, a blood transfusion may be necessary.
The alteration of nipple sensitivity is almost unavoidable, it will gradually get back within a few months.
Necrosis: it is the loss of a more or less large skin zone that can affect cosmetics results (loss of skin), loss of the nipple. Tobacco smoking may be aggravating. This is why it is most recommended to stop smoking at least three weeks before and after surgery. In case of necrosis, an additional complementary surgical act may be necessary afterward (one year).